A Post-Antibiotic World
Antibiotic-resistant bacteria infect more than 2 million people in the U.S. each year. Are we smarter than bacteria?
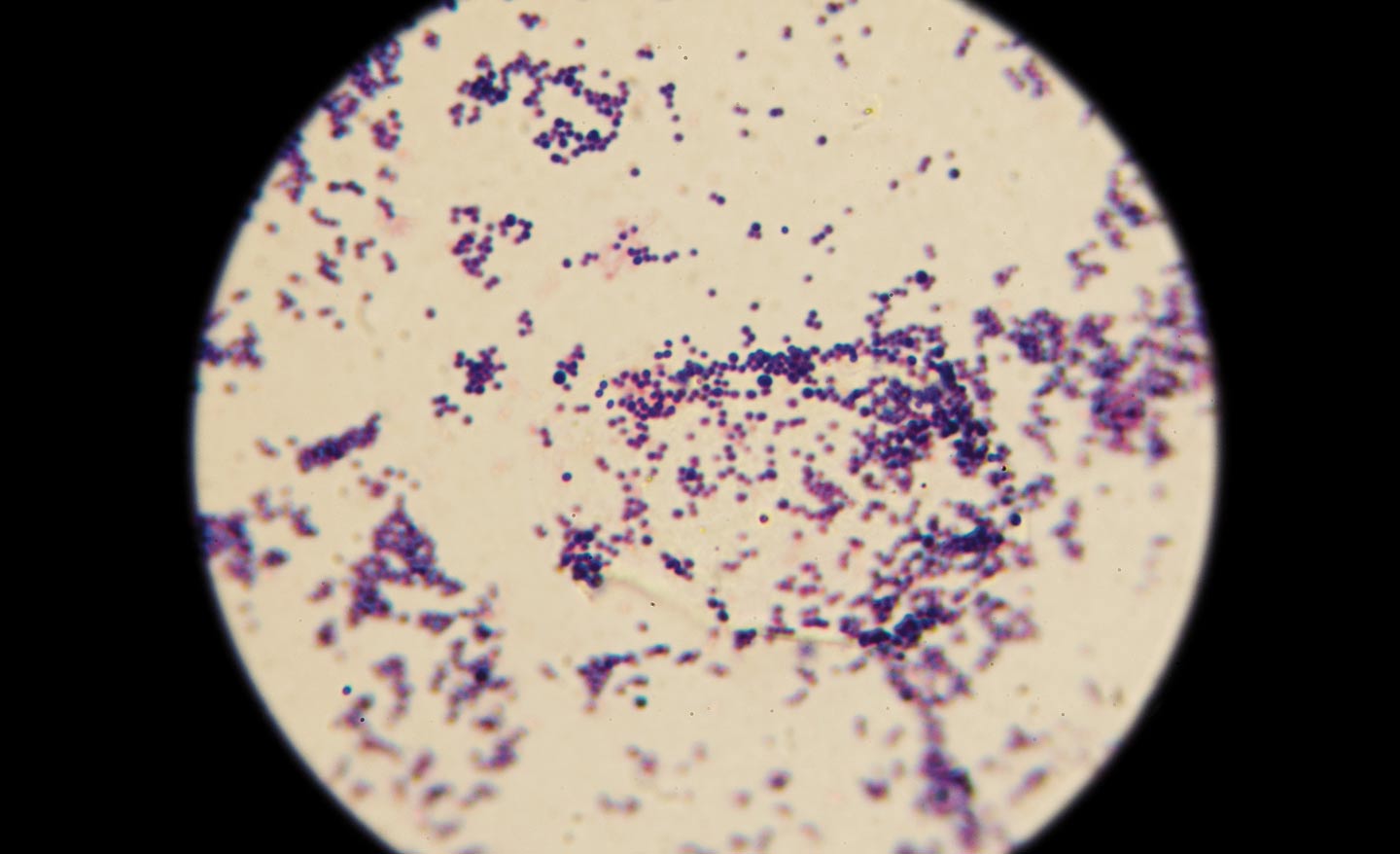
Bacteria kill.
Each year in the U.S., antibiotic-resistant bacteria infect more than 2 million people, and at least 23,000 die as a result of these infections. And many more patients die from conditions complicated by antibiotic-resistant infections, according to the Centers for Disease Control and Prevention.
The culprits range from bacteria—including methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile (C. difficile), which escape hospitals and invade local gyms, schools and playgrounds— to the pathogens labeled as “priority one critical” by the World Health Organization: Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacteriaceae.
In fact, some scientists currently argue that we’re quickly approaching a post-antibiotic world where even simple surgeries risk infections that cannot be quashed by the big-gun antibiotics methicillin or vancomycin. Because bacteria are constantly evolving to fight antibiotics as well as our body’s own immune system, the worry becomes that a time will come where everyday infections begin to kill us.
The good news, says Tanya Schneider, associate professor of chemistry, is that “we are smarter than bacteria.”
Schneider is a chemist who, unlike a microbiologist who looks at different bacteria, focuses on the problem at the molecular level.
“I’m really looking at the molecular details, the molecules made by bacteria,” Schneider says.
Schneider researches quorum-sensing molecules—the way in which bacteria communicate by producing small molecules in their local environment—specifically Pseudomonas aeruginosa, a Gram-negative problematic human pathogen. This pathogen (Conn does not have it in its labs) is particularly problematic in immunocompromised people, patients with cancer, severe burns or AIDS. The pathogen is extremely dangerous for patients with cystic fibrosis.
“I was motivated in part to study this organism because it colonizes lungs of cystic fibrosis patients, and I have family friends whose son died of cystic fibrosis,” Schneider says.
“[The pathogen is] difficult to get rid of, but doesn’t necessarily impact the general population. But in a hospital setting this can be termed a superbug.”
Antibiotics are an effective way to kill bacteria. But this usage also promotes the selective pressure on the bacterial community to evolve into what are called superbugs. Antibiotic resistance, of course, arises from overprescription and incorrect usage and from an abundance of antibiotics creeping into our food supply.
Superbugs, Schneider says, develop because bacteria grow and divide so quickly. Eventually, if one colony of bacteria isn’t killed by an antibiotic that colony will grow, divide and survive, forming a resistance to antibiotics.
During this process, bacteria stave off death by adapting. To inhibit antibiotic resistance, scientists are working toward pharmaceuticals that wound—rather than kill—bacteria, leaving the body’s own immune system to fight off the wounded bug. Not faced with obliviation, bacteria will not be threatened to the point where they must fight to survive. Part of Schneider’s research is to track ways to inhibit growth of bacteria rather than kill them.
“As a bacterial colony grows and produces more signaling molecules, other neighboring bacteria detect their presence. The goal is to increase understanding of bacterial enzymes that enable the production of the signaling molecules in order to inhibit their activity,” Schneider says.
“We’re interested in what we might call bacteriostatic, something that slows down or minimizes bacterias’ ability to grow, rather than bacteriocidal, which is killing them.”